Allergy? Intolerance? What’s the difference?

With hospital admissions for children with severe allergic reactions (anaphylaxis) doubling over the past decade, and with one in ten children living with a food allergy or sensitivity, the “allergy issue” and how to manage it is something every early childhood education and care (ECEC) setting will have to face at one time or another.
When children living with allergy or anaphylaxis are within your care, it’s important to understand the problem and have clear guidelines on how to manage their allergies and sensitivities when preparing and serving meals.
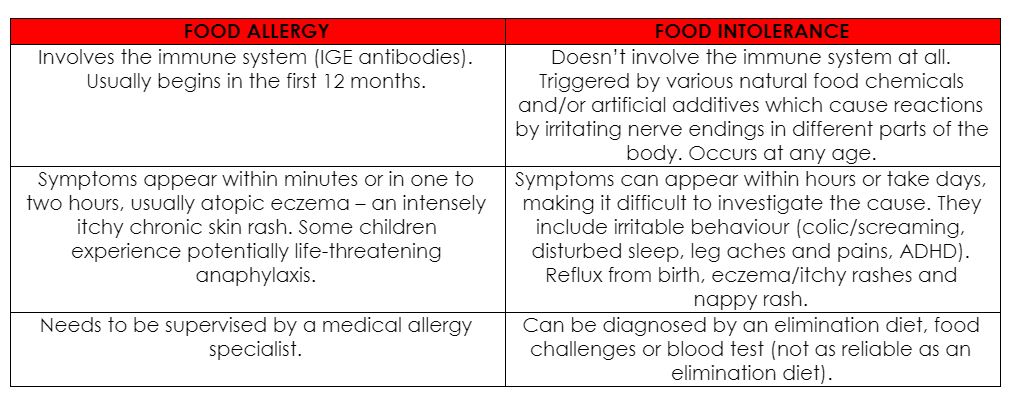
The difference between food allergies and food intolerances
It’s more common these days to see children with a growing list of food intolerances. Although the symptoms can cause discomfort, food intolerances do not involve the immune system and are not life-threatening.
Food intolerances are often caused by food chemicals, which are naturally occurring in foods such as food additives e.g. monosodium glutamate (MSG); enzyme deficiencies such as lactose intolerance, and unexplained causes.
The main symptoms include:
- Hives
- Reflux
- Bloating
- Cramping
- Constipation
- Diarrhea
- Mouth ulcers
- Headaches
- Irritability
Why do food allergies occur?
Allergies occur when the body overreacts to an allergen or ‘trigger’ that is typically harmless to most people. Around one person in four is allergic to something, and around half of all allergy sufferers are children. The symptoms of an allergy range from mild to severe. The most severe type of allergic reaction is anaphylaxis, which can be fatal if prompt medical attention is not sought. However, in most cases, effective treatments are available to manage or treat allergy symptoms.
What are the symptoms?
Common signs that a child may have an allergy include sneezing; a runny nose; red, watery, itchy eyes; wheezing, coughing and problems breathing; tongue swelling; headaches; skin rashes; tummy pains, vomiting and diarrhea; and, hypotension and collapse. Food allergies, in particular, are often associated with hives or swelling around the mouth, which usually happens within 30 minutes of ingesting a food the child is allergic to.
How to avoid or manage food allergies in a childcare setting
It’s essential that leaders, educators and chefs have detailed guidelines and action plans on how to manage allergies in a childcare setting.
It is common to see children with food allergies receiving repetitive or less nutritious meals due to a lack of knowledge on how to create nutritious substitutes. The Wholesome Child Nourish program ensures children receive the nutrients they need to thrive, despite their allergies or intolerances.
The main food allergies
There are nine foods that are largely responsible for more than 90 per cent of food allergies:
- Cow’s milk
- Egg
- Peanut
- Tree nuts
- Fish
- Shellfish
- Soy
- Wheat
- Sesame
When children have a dairy allergy, for example, it is important to ensure they still receive sufficient calcium by providing non-dairy alternatives that are calcium rich, such as canned sardines and salmon, basil, kale, poppy, sesame and chia seeds. There’s also tahini, tofu and broccoli to increase variety – all important and healthy calcium-rich additions.
Food allergies can develop at any age but are most common in children less than five years old. Even young babies can develop food allergy symptoms.
Eggs, milk and peanuts are the three most common allergenic foods for infants. An infant who already has a milk or egg allergy is known to be at risk for later developing a peanut allergy. Another risk factor associated with a peanut allergy is moderate to severe eczema (atopic dermatitis).
What to do?
If you suspect a child has a food allergy or intolerance, it is best to speak to parents about seeing their GP or pediatrician as soon as possible. It can also help to do the following:
- Keep a food diary and record food eaten and any reactions. Include what food was eaten, how much, what symptoms, how long they lasted and if any medication was given.
- If a reaction occurs in your centre, speak to the chef/cook to find out exactly what was in the food given to your child.
- If a symptom arises – such as a rash – take a photograph to share with parents and their doctor.
- If a symptom occurs after eating a particular packaged food, save the packaging with the nutrition label or take a photo for parents.
- Work with parents and their doctor to remove suspected foods from the diet for a period of two to six weeks or until symptoms fade.
- Slowly reintroduce the foods, in a controlled manner, one at a time, recording any symptoms if they should appear.
Give parents the confidence to send their children to your setting, knowing your team understands their child’s needs and can accommodate them with diligence while still providing nourishing food.
Popular

Workforce
Policy
Quality
Practice
Provider
Research
ECEC must change now, our children can’t wait for another inquiry
2025-07-02 07:47:14
by Fiona Alston

Practice
Provider
Quality
Workforce
Leading with Curiosity: How distributed leadership is redefining the future of early childhood education
2025-07-03 07:42:07
by Contributed Content

Events News
Workforce
Marketplace
Practice
Quality
Provider
Research
An exclusive “Fireside Chat” with ECEC Champion Myra Geddes
2025-07-01 11:25:05
by Fiona Alston













