Advocacy
Compliance
In The Field
Allergy? Intolerance? What’s the difference?
Mandy Sacher
Oct 30, 2019
Save
With hospital admissions for children with severe allergic reactions (anaphylaxis) doubling over the past decade, and with one in ten children living with a food allergy or sensitivity, the “allergy issue” and how to manage it is something every early childhood education and care (ECEC) setting will have to face at one time or another.
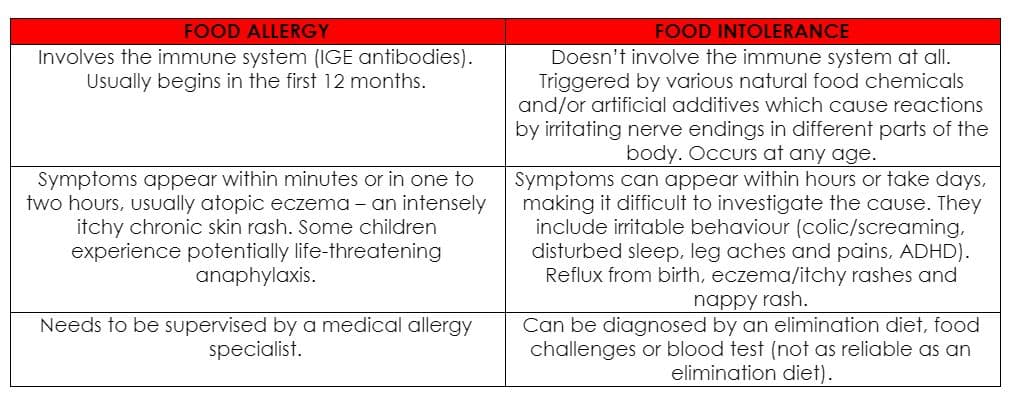
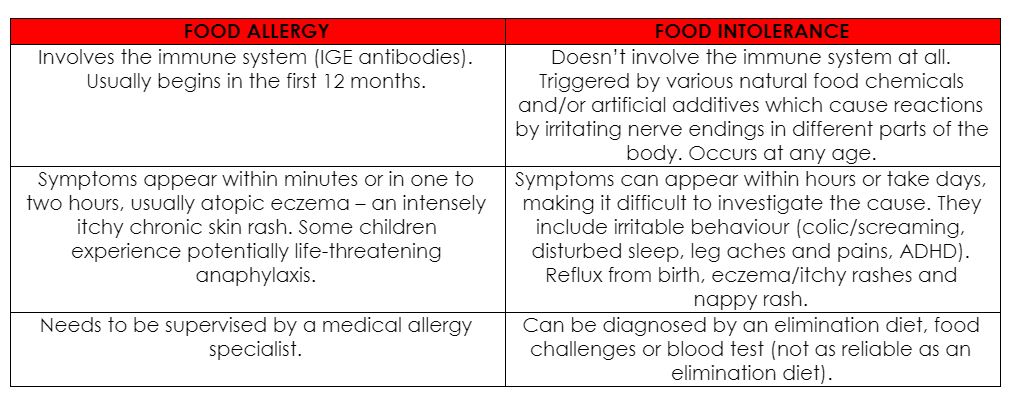
When children living with allergy or anaphylaxis are within your care, it’s important to understand the problem and have clear guidelines on how to manage their allergies and sensitivities when preparing and serving meals.The difference between food allergies and food intolerancesIt’s more common these days to see children with a growing list of food intolerances. Although the symptoms can cause discomfort, food intolerances do not involve the immune system and are not life-threatening.
Food intolerances are often caused by food chemicals, which are naturally occurring in foods such as food additives e.g. monosodium glutamate (MSG); enzyme deficiencies such as lactose intolerance, and unexplained causes.
The main symptoms include:
- Hives
- Reflux
- Bloating
- Cramping
- Constipation
- Diarrhea
- Mouth ulcers
- Headaches
- Irritability
 Why do food allergies occur?Allergies occur when the body overreacts to an allergen or ‘trigger’ that is typically harmless to most people. Around one person in four is allergic to something, and around half of all allergy sufferers are children. The symptoms of an allergy range from mild to severe. The most severe type of allergic reaction is anaphylaxis, which can be fatal if prompt medical attention is not sought. However, in most cases, effective treatments are available to manage or treat allergy symptoms.
Why do food allergies occur?Allergies occur when the body overreacts to an allergen or ‘trigger’ that is typically harmless to most people. Around one person in four is allergic to something, and around half of all allergy sufferers are children. The symptoms of an allergy range from mild to severe. The most severe type of allergic reaction is anaphylaxis, which can be fatal if prompt medical attention is not sought. However, in most cases, effective treatments are available to manage or treat allergy symptoms. What are the symptoms?Common signs that a child may have an allergy include sneezing; a runny nose; red, watery, itchy eyes; wheezing, coughing and problems breathing; tongue swelling; headaches; skin rashes; tummy pains, vomiting and diarrhea; and, hypotension and collapse. Food allergies, in particular, are often associated with hives or swelling around the mouth, which usually happens within 30 minutes of ingesting a food the child is allergic to.
How to avoid or manage food allergies in a childcare settingIt’s essential that leaders, educators and chefs have detailed guidelines and action plans on how to manage allergies in a childcare setting.
It is common to see children with food allergies receiving repetitive or less nutritious meals due to a lack of knowledge on how to create nutritious substitutes. The Wholesome Child Nourish program ensures children receive the nutrients they need to thrive, despite their allergies or intolerances.
The main food allergiesThere are nine foods that are largely responsible for more than 90 per cent of food allergies:
- Cow’s milk
- Egg
- Peanut
- Tree nuts
- Fish
- Shellfish
- Soy
- Wheat
- Sesame
When children have a dairy allergy, for example, it is important to ensure they still receive sufficient calcium by providing non-dairy alternatives that are calcium rich, such as canned sardines and salmon, basil, kale, poppy, sesame and chia seeds. There’s also tahini, tofu and broccoli to increase variety – all important and healthy calcium-rich additions.
Food allergies can develop at any age but are most common in children less than five years old. Even young babies can develop food allergy symptoms.
Eggs, milk and peanuts are the three most common allergenic foods for infants. An infant who already has a milk or egg allergy is known to be at risk for later developing a peanut allergy. Another risk factor associated with a peanut allergy is moderate to severe eczema (atopic dermatitis).
What to do?If you suspect a child has a food allergy or intolerance, it is best to speak to parents about seeing their GP or pediatrician as soon as possible. It can also help to do the following:
- Keep a food diary and record food eaten and any reactions. Include what food was eaten, how much, what symptoms, how long they lasted and if any medication was given.
- If a reaction occurs in your centre, speak to the chef/cook to find out exactly what was in the food given to your child.
- If a symptom arises – such as a rash – take a photograph to share with parents and their doctor.
- If a symptom occurs after eating a particular packaged food, save the packaging with the nutrition label or take a photo for parents.
- Work with parents and their doctor to remove suspected foods from the diet for a period of two to six weeks or until symptoms fade.
- Slowly reintroduce the foods, in a controlled manner, one at a time, recording any symptoms if they should appear.
Give parents the confidence to send their children to your setting, knowing your team understands their child’s needs and can accommodate them with diligence while still providing nourishing food.
Don’t miss a thing
Related topics
Compliance
Changes
Advocacy
Leadership
In The Field
Understanding Children
Marketplace
Products
General News
Legislation
Affordability & Accessibility
Politics
Innovative Research
Allied Fields
Professional development
Family Day Care
Long Day Care
NQF and Policy Changes
Outside School Hours Care
Preschool
Property
Report Summaries
Examples
Reporting
Services
Personnel Appointments
Events News
Jobs News
Other
Corporate activity


















